Oh What A Night
Last night was a night to remember...I know I keep on saying things like, "Last call was one for the ages!"...but in all seriousness I will not be forgetting the events of last night's call any time in the near future...
The situation: A patient who has been gradually getting worse over the course of the past 2-3 days--we think she has some kind of infection, just haven't figured out what yet--decides to stop breathing at about 1 in the morning. The standard practice in such a situation is to perform endotracheal intubation: sticking a tube down somebody's trachea, then hooking that tube up to a ventilator in order to let the machine take over the process of breathing. The hope of course is that it's a temporary measure--once you figure out how to get the patient reliably ventilating on their own again, you eventually wean them off the ventilator.
In any case, we had problems ventilating her on the breathing machine from the get-go. Usually you would try and push breaths in at a volume of about 400 cc's (same thing as 400 milliliters) of air with each breath. However, her lungs were stiff as a board--we were only able to move about 100 c's of air in with each breath--which would be incompatible with life if allowed to go on indefinitely! Why were we having so much trouble ventilating? A frantic search was turning up few answers...the machine seemed to be hooked up correctly...we got a stat chest X-ray and it looked like the endotracheal tube was in the right place...there was no pneumothorax (a collapsed lung due to the inadvertant puncturing of the lining of the lung)...all the meanwhile, her blood pH was heading down to critically low levels. Normally the acid in your blood is kept in a very narrow range of 7.35-7.45. Her pH was down to 6.88 at one point, an indication that we were not ventilating her adequately...
Fortunately, an answer revealed itself...on physical exam she had an abdomen that was rock hard--you pressed down on her belly and instead of being nice and soft it was markedly distended and felt like a gigantic mushy mass was filling up the entire peritoneum. So much so, in fact, that the reason the lungs weren't allowed to expand was because they simply couldn't inflate past the pressure being exerted on themselves by whatever was going on in the abdomen. But what the hell was it? We rolled our handy-dandy portable ultrasound machine over to the bedside and took a glance...it was fluid! Just liters and liters of fluid which had leaked out from her blood vessels and eventually into the peritoneum.
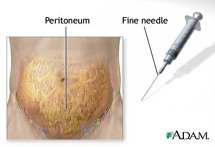 Postulating that she had something called "intra-abdominal compartment syndrome"--basically, that the large amounts of fluid was creating such massive amounts of pressure, they were not allowing the lungs to expand--we performed an emergent paracentesis at her bedside. This consisted of me plunging a relatively small, 19-gauge needle into the fluid and draining out about 2 Liters of the straw-colored liquid into bottles. The response was dramatic! Her tidal volumes of only 100 cc's instantly started increasing...first to 150...then to 200...then 300...then up to a healthy 400 cc's! Before long she was adequately ventilating, and by the morning her pH was actually within the normal range. Whew!
Postulating that she had something called "intra-abdominal compartment syndrome"--basically, that the large amounts of fluid was creating such massive amounts of pressure, they were not allowing the lungs to expand--we performed an emergent paracentesis at her bedside. This consisted of me plunging a relatively small, 19-gauge needle into the fluid and draining out about 2 Liters of the straw-colored liquid into bottles. The response was dramatic! Her tidal volumes of only 100 cc's instantly started increasing...first to 150...then to 200...then 300...then up to a healthy 400 cc's! Before long she was adequately ventilating, and by the morning her pH was actually within the normal range. Whew!
Problem solved? Yes and no. If she had gone on for another 10-20 minutes, I believe she would have likely died. So we prevented her from dying that night. However there are still a whole host of other problems which still need to be addressed (such as why all that fluid was in her belly in the first place). The ICU is a very humbling place to be...
In addition to the above fireworks, my intern was The Man yesterday when it came to procedures. While it was I who had the glory of performing the emergent paracentesis, he came through in spades with two successful spinal taps, an expertly-placed central line, and a (non-emergent) paracentesis of his own. And on his birthday, no less!
Day off tomorrow...should be nice to decompress a little...


0 Comments:
Post a Comment
<< Home